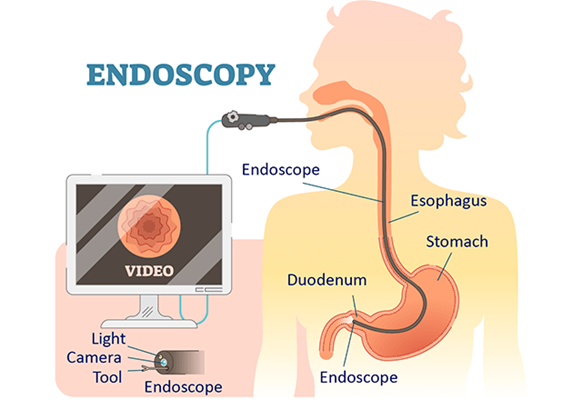
Upper GI endoscopy is a visual examination of the upper intestinal tract using a lighted, flexible tube camera. The upper gastrointestinal endoscopy examines the upper part of gastrointestinal tract oesophagus,stomach and Duodenum.
This videoendoscope has a tiny, optically sensitive computer chip at the end which transfers signals to a large video screen. An open channel in these scopes allows other instruments to be passed through in order to take tissue samples, remove polyps and perform other exams.
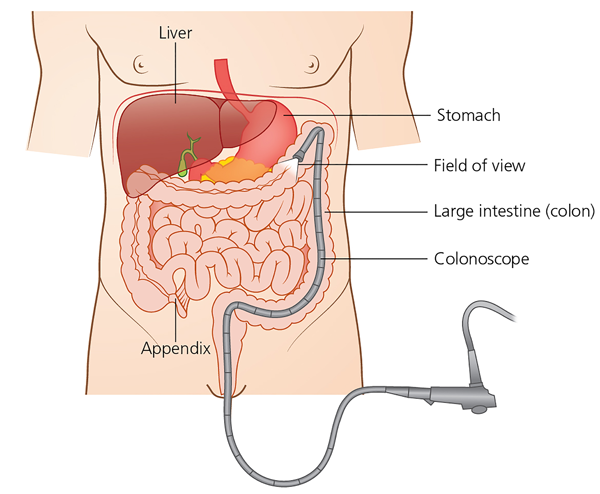
Colonoscopy is the examination of Large intestine with a slim, flexible & lighted tube. Passed through the back passage. This is done with mild sedation.
laparoscopy surgery done in hospital
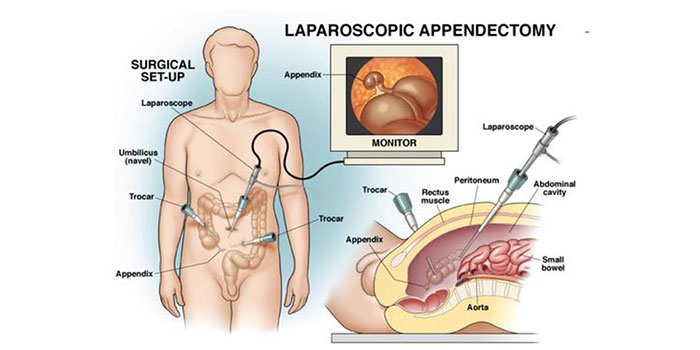
Appendicitis is an inflammation of the appendix, a small, fingerlike tube that hangs from the lower right side of the large intestine. The purpose of the appendix is not known. It usually becomes inflamed because of an infection or an obstruction in the digestive tract. If untreated, an infected appendix can burst and spread the infection throughout the abdominal cavity and into the bloodstream.
The risk of appendicitis increases with age, peaking between ages 15 and 30. Appendicitis is the main reason for abdominal surgery in children.

If you have symptoms of appendicitis, do not take enemas or laxatives to relieve constipation: These medicines increase the chance that the appendix will burst. Also, avoid taking pain-relief medicines before seeing your doctor, because these medications can mask appendicitis symptoms and make diagnosis difficult.
Your doctor will examine you and check for pain in your lower right abdomen.After the physical examination, your doctor will order blood tests to check for signs of infection and a urinalysis to rule out a urinary tract problem. Your doctor may order an ultrasound or computed tomography (CT) scan to help confirm the diagnosis.
Most people will seek medical attention within 12 to 48 hours because of the abdominal pain. In some cases, a low level of inflammation exists for several weeks before a diagnosis is made.
There is no way to prevent appendicitis.
The standard treatment is to remove the appendix. The surgery, called an appendectomy, should be done as soon as possible to reduce the risk of the appendix rupturing. If appendicitis is strongly suspected, a surgeon will often advise removing the appendix even if an ultrasound or CT scan cannot confirm the diagnosis. The surgeon’s recommendation to operate reflects the danger of a ruptured appendix: It can be life threatening, while an appendectomy is a relatively low-risk operation. In most laparoscopic appendectomies, surgeons operate through 3 small incisions (each ¼ to ½ inch) while watching an enlarged image of the patient’s internal organs on a television monitor. In some cases, one of the small openings may be lengthened to complete the procedure.
Cholecystectomy is the surgical removal of the gallbladder, the small saclike organ located near the liver in the upper right side of the abdomen. It is attached to the main duct that carries bile from the liver into the intestine. Bile helps your body to break down and absorb fats. The gallbladder temporarily stores bile from the liver. There are two ways to remove the gallbladder:
Surgeons remove gallbladders to prevent complications from gallstones, which are rocklike lumps that form inside the gallbladder. Gallstones can cause symptoms as simple as intermittent crampy pain after eating, but they also can lead to cholecystitis, cholangitis, or pancreatitis.
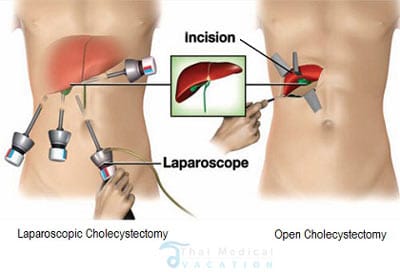
The surgeon cuts open the abdomen and removes the gallbladder through an incision that is about 6 inches long. The abdomen is then stitched closed again.
The surgeon cuts open the abdomen and removes the gallbladder through an incision that is about 6 inches long. The abdomen is then stitched closed again.
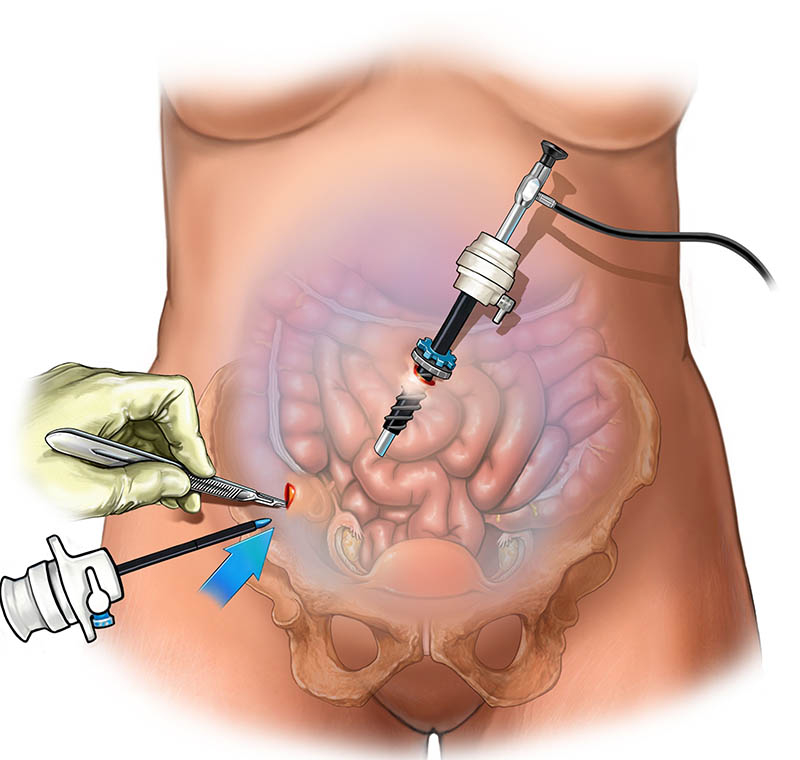
The surgeon makes a small incision at the navel and puts air into the abdomen to make it easier to see. This help to avoid damaging any organs with the incisions or instruments. Next the laparoscope is inserted through the small incision at your navel. Once the laparoscope is inside your abdomen, a camera on the laparoscope transmits images to a viewing screen. Three smaller incisions are made, and the surgical instruments are inserted through these incisions. The surgeon cuts out the gallbladder, and removes the gallbladder through one of the incisions, usually the one at your bellybutton. All of the instruments are removed, and the surgeon closes the incisions with stitches or surgical tape. You may be able to eat a light meal later that day (in the evening). Sometimes patients stay in the hospital until the next morning.
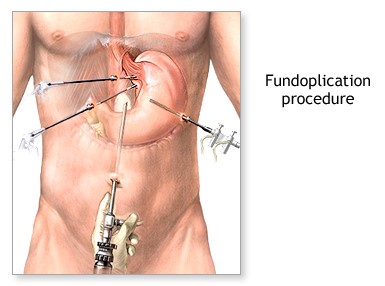
GERD is a chronic disease where the acidic contents of the stomach get refluxed into the lower esophagus, thereby causing damage to it.
Surgeons remove gallbladders to prevent complications from gallstones, which are rocklike lumps that form inside the gallbladder. Gallstones can cause symptoms as simple as intermittent crampy pain after eating, but they also can lead to cholecystitis, cholangitis, or pancreatitis.
The surgeon cuts open the abdomen and removes the gallbladder through an incision that is about 6 inches long. The abdomen is then stitched closed again.
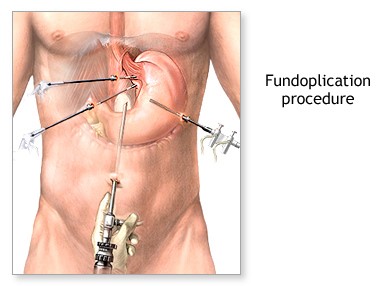
Caused by damage or abnormalities in the barrier between the esophagus and stomach
Abnormal relaxation in the sphincter muscles that help seal off the stomach Impaired expulsion of the acidic, semi-digested content from the stomach or esophagus
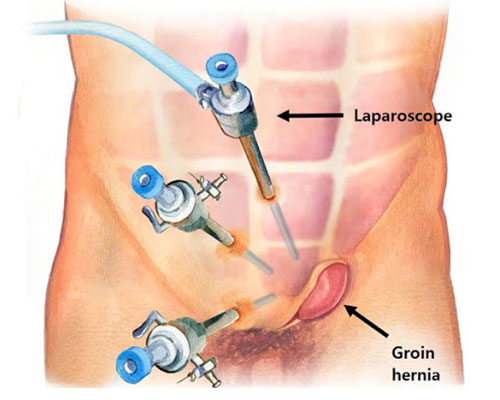
A few incisions are made in the abdomen area, through which tiny tube shaped instruments are inserted. A laparoscope which has a tiny video camera and a powerful light source is then inserted through this incision to allow the doctor to view the procedure on a monitor. Another incision is used to insert surgical instruments in the body by which the procedure is carried out. It is performed under general anesthesia.
A Hernia is caused when the supporting, internal tissues of an organ start to bulge out of the weakened abdominal wall where they are normally contained. It is a small balloon-like sac that occurs when the inner lining of the abdominal muscle pushes its way through the abdominal wall due to an opening or weakness of the wall.
The surgeon cuts open the abdomen and removes the gallbladder through an incision that is about 6 inches long. The abdomen is then stitched closed again.
The laparoscopic procedure for repairing hernia is the latest and most advanced procedure for correcting hernia In this procedure, a laparoscope (a telescope connected to a camera and other surgical instruments) is inserted through micro incisions to allow the surgeon to get a clear, high-resolution image of the hernia and its surrounding tissues
Hemorrhoidectomy is surgery to remove hemorrhoids. You will be given general anesthesiaor spinal anesthesia so that you will not feel pain.
Incisions are made in the tissue around the hemorrhoid. The swollen vein inside the hemorrhoid is tied off to prevent bleeding, and the hemorrhoid is removed. The surgical area may be sewn closed or left open. Medicated gauze covers the wound.
Surgery can be done with a knife (scalpel), a tool that uses electricity (cautery pencil), or alaser. The operation is usually done in a surgery center. You will most likely go home the same day (outpatient).
There is a procedure that uses a circular stapling device to remove hemorrhoidal tissue and close the wound. No incision is made. In this procedure, the hemorrhoid is lifted and then "stapled" back into place in the anal canal. This surgery is called stapled hemorrhoidopexy. People who have stapled surgery may have less pain after surgery than people who have the traditional hemorrhoid surgery. But the stapled surgery is more expensive.
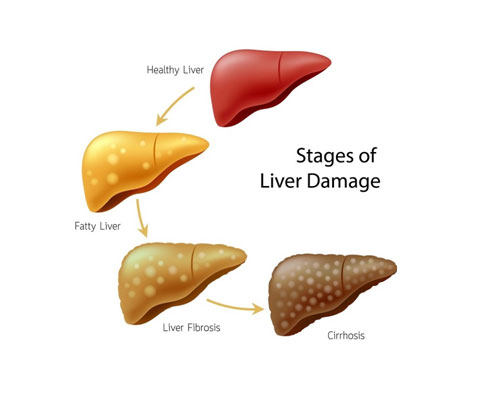
The liver is the largest solid organ in the human body. Also, it performs more than 500 functions in the body. These functions include detoxification, production of chemicals that help in the digestion of food. The liver disease could be fatal and one should immediately look for treatment.
The liver is an essential organ in the gastrointestinal tract that helps in food digestion and freeing the body from toxic elements.
If you sense any liver-related disorder symptoms earlier, it can lead to liver cirrhosis – a life-threatening condition. But treating earlier can save the liver timely.
There are a variety of health conditions that are responsible for causing liver diseases and they are:
When an individual consumes alcohol in excess, it leads to:
Upon experiencing any liver disease-related symptoms, your doctor may perform evaluation tests to diagnose the cause and extent of the liver disease. These tests may include:
The liver is the only organ in the body that can regenerate damaged cells by itself. There are various methods to treat liver damage depending on its diagnosis, severity, stage, size, and location. The treatment options may include:
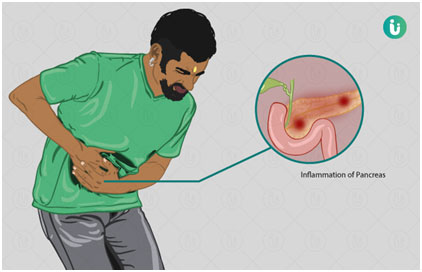
Pancreatitis is a disease in which your pancreas becomes inflamed. The pancreas is a large gland behind your stomach and next to your small intestine. Your pancreas does two main things:
Your pancreas can be damaged when digestive enzymes begin working before your pancreas releases them.
The two forms of pancreatitis are acute and chronic
If you have an attack of acute pancreatitis, you may receive strong drugs for pain. You may have to have your stomach drained with a tube placed through your nose. If the attack is prolonged, you may be fed and hydrated intravenously (through a vein).
You’ll probably need to stay in the hospital, where your treatment may include: